Marketing and Empathy Psychology
Ultimate Guide to CMS Compliance: Discharge Planning, Telemedicine, and Nursing Standards
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.
Tab #1
Tab #2
Tab #2
Tab #1
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.
Tab #2
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.
Tab #2
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.
Discharge Planning Compliance
CMS Swing Bed Requirements
Medical Staff & Telemedicine Requirements
Nursing CMS CoP Standards
Discharge Planning Compliance
Discharge Planning: Compliance with CMS Hospital & CAH CoPs
- DURATION : 60
- DATE / TIME(EST) : August 21, 2024 | 1:00 pm
- SPEAKER : Laura A. Dixon, BS, JD, RN, CPHRM
Overview
Every hospital that accepts Medicare and Medicaid must comply with the CMS discharge planning guidelines. These standards must be followed for all patients and not just Medicare or Medicaid. CMS requires several discharge planning policies and procedures so learn which ones are required and why
CMS published changes to the discharge planning standards in February 2020, but has yet to publish revised interpretive guidelines and survey procedures to match the new regulations.
This program will discuss the Impact Act and how it affects hospital discharge planning. It requires standardized assessment, quality data, and resource data requirements. It requires hospitals to assist patients with post-discharge care such as home health, skilled nursing facilities, long term care hospitals and inpatient rehab facilities. Patients have freedom of choice and now information on all four must be provided to the patient except for CAHs.
The new regulations cover sections on patient timely access to medical records, the discharge planning process, discharge instructions, discharge planning requirements. It will cover transfers to other facilities, assessment of readmission within 30 days, caregiver rights and recommendations, reduction of factors that lead to preventable readmissions, timely discharge planning, and more.
Discharge Planning Conditions of participation for Critical Access hospitals will be discussed briefly. Those regulations follow the Acute hospitals requirements.
Objectives/Outcomes
- Discuss the CMS has revised the discharge planning requirements that apply to all hospitals and critical access hospitals
- Recall patients and physicians can request a discharge planning evaluation
- Discuss that information about the hospitalization must be provided to the physician or provider before the first post hospital visit
- Describe that the patient has a right to get medical records timely including a copy of their discharge plan
Agenda
- Introduction
- Deficiency data for discharge planning
- Discharge planning process and the IMPACT Act
- Identification of patients needing discharge planning
- Role of support person
- Incapacitated patient
- Discharge planning process
- RN, social worker, or qualified person to develop evaluation
- Timely evaluation
- Discussion of evaluation with patient or individual acting on their behalf
- Discharge evaluation in the medical record
- Documentation of the discharge process
- Discharge plan
- Physician request for discharge planning
- Implementation of the patient’s discharge plan
- Reassessment of the discharge plan
- Freedom of choice for post-acute care providers
- Transfer or referral
- Critical Access Hospital Discharge planning requirements
- Discharge planning metrics
- Appendix and Resources
- Resources and internet links
Who Should Attend?
- Discharge planners
- Transitional care nurses
- Social workers
- All staff nurses who discharge patients in a hospital setting
- Chief nursing officer
- Nurse educators
- Chief operation officer
- Chief medical officers
- Physicians
- Risk managers
- Regulatory/Compliance officer
- UR nurses
- Joint Commission coordinator
- Chief executive officer
- Nurse managers
- PI director
- Health information director
- Patient safety officer
- Any person serving on a hospital committee to redesign the discharge process to prevent unnecessary readmissions.
CMS Swing Bed Requirements
CMS CAH Swing Bed Requirements
- DURATION : 60
- DATE / TIME(EST) : August 21, 2024 | 1:00 pm
- SPEAKER : Laura A. Dixon, BS, JD, RN, CPHRM
Overview
Swing Beds can be a financial lifeline for Critical Access Hospitals. This webinar will focus on swing bed regulations in Appendix W for Critical Access Hospitals. Interpretive guidelines and survey procedures are under Appendix PP – Long Term Care manual, which will be discussed in the corresponding regulation sections.
It is challenging to figure out what the interpretive guidelines and survey procedures are as there is there was no crosswalk between Appendix W – for CAH – and Appendix PP – Long Term Care. This webinar was created to assist hospitals in understanding what needs to be done.
Also to be discussed will be common deficiencies involving swing beds and how to avoid them.
Objectives
- Discuss the requirements for a patient to be admitted to Swing Bed status
- Recall how to locate the regulation and interpretive guidelines and survey procedures for swing beds
- Describe what is required by CMS to be in the resident assessment which is done to do the care plan
- Recall the CMS requirements for emergency dental care for swing bed patients
Agenda
Manual and Introduction to CAH CoPs
- Introduction
- How to Locate the Manual
- Common Swing Bed deficiencies
Special Requirements for CAH Providers of Long-Term Care Services (Swing beds)
- Introduction to Swing Beds
- Interpretive guidelines and survey procedure under Appendix PP
- Eligibility
- Payment
- Healthcare literacy
- SNF Services
- Patient/Resident Rights
- Exercise of Rights
- Notice of Rights and Services
- Free Choice
- Privacy and Confidentiality
- Work
- Access and Visitation Rights
- Personal Property
- Married Couples
- Admission, Transfer and Discharge Rights
- Transfer and Discharge
- Payment of care
- Content of notice
- Resident Behavior and Facility Practices
- Restraints, Abuse
- Staff Treatment of Residents
- Hiring of employees
- Patient Activities
- Social Services
- Dental requirements change
- Resident Assessment
- Comprehensive Care Plans
- PASARR or RAI
- Trauma informed care
- Discharge Summary
- Nutrition
Appendix and Resources
Who Should Attend?
- CEO
- COO
- CFO
- Nurse executives
- Accreditation and Compliance/Regulation director
- Nurse managers
- Pharmacists
- Quality managers
- Risk managers
- Health information management personnel
- Social workers
- Dieticians
- Nurses
- Nurse educators
- Nursing supervisors
- Patient safety officer
- Director of Rehab (OT, PT, speech pathology, and audiology)
- Infection preventionist
- Anyone who is responsible for care of swing bed patients in a CAH
- Persons responsible implementing the CMS swing bed requirements
Medical Staff & Telemedicine Requirements
Medical Staff and Telemedicine: Meeting CMS Conditions of Participation and the Joint Commission Standards
- DURATION : 60
- DATE / TIME(EST) : August 21, 2024 | 1:00 pm
- SPEAKER : Laura A. Dixon, BS, JD, RN, CPHRM
Overview
Any hospital that accepts Medicare and Medicaid payments must comply with the regulations known as Conditions of Participation. The Centers for Medicare and Medicaid Services (CMS) hospital CoPs have sections on all aspects of patient care including medical staff and telemedicine.
The medical staff section includes information on credentialing and privileging requirements, implementing Medical Staff (MS) bylaws and rules and regulations, hospitals in systems.
The Governing Body and Medical Staff sections in the Manual will be discussed in relation to medical staff requirements and oversight. There will also be a concurrent discussion of TJC standards for medical staff.
Although telemedicine has been a factor in healthcare for many years, COVID-19 gave it a larger role in diagnosis and treatment of patients. Every hospital and critical access hospital that participate in or utilize telemedicine should ensure compliance.
The regulations cover the credentialing and privileging process for physicians and practitioners providing telemedicine services to another hospital. This revised process is less burdensome for hospitals, so CMS allows hospitals to credential such providers by proxy. Hospitals are required to have a written agreement that meets certain criteria. This webinar will briefly cover important provisions that should be considered in a telemedicine contract.
Objectives
- Recall that hospitals can have a separate medical staff or a unified shared integrated medical staff
- Describe the requirements for a medical staff under CMS Conditions of Participation and TJC standards
- Describe the requirement that hospitals must have a written telemedicine agreement specifying the responsibilities of the distant-site hospital and entities to meet the required credentialing requirements
- Recall that Joint Commission has standards on telemedicine
Detailed Outline
- Introduction to the Manual
- Deficiencies – Medical Staff and Telemedicine
- Overlap of Governing Board and Medical Staff sections
- Appointment of individuals to the MS
- Unified and integrated staff
- Eligibility and appointment
- Periodic appraisals
- Credentialing
- Organization and accountability
- Hospital systems
- Medical Staff bylaws
- Medical staff duties
- History & physicals
- Advanced practice providers and H&Ps
- Critical Access Hospitals Medical staff
- Professional and ancillary staff
- Review of professional services
- Additional considerations for medical staff
- TJC Standards for Medical Staff
- Telemedicine introduction and definitions
- Distant site telemedicine hospital
- Distant site entity (DTSE)
- Requirement for written agreement for Telemedicine
- Telemedicine privileges based on medical staff recommendations
- Credentialing by proxy
- Agreements with Medicare certified hospitals
- Agreements with telemedicine entities
- Adverse events and notification
- Periodic appraisals
- Complaints received about the distant site physician
- Joint Commission telemedicine standards
- Suggested content for telemedicine agreements
- Telemedicine resources
- Appendix & Resources
Who Should Attend?
- Chief Medical Officer
- Medical Staff leader
- Credentialing and Privileging Professionals
- Physicians
- Medical staff office staff and coordinator
- Teleradiology Professionals
- Chief Nursing Officer
- Chief Operating Officer
- Risk manager
- Compliance officer – CMS and/or TJC/DNV
- Patient safety officer
- Nurse educator
- Accreditation Director
- Director of Regulatory Affairs
- Telemedicine director
- Anyone involved or in contracting for telemedicine services
Nursing CMS CoP Standards
Nursing: CMS CoP Standards for Hospitals
- DURATION : 60
- DATE / TIME(EST) : August 21, 2024 | 1:00 pm
- SPEAKER : Laura A. Dixon, BS, JD, RN, CPHRM
Overview
Every hospital that accepts Medicare and Medicaid reimbursement must follow the CMS (Center for Medicare and Medicaid Services) Conditions of Participation (CoPs) and it must be followed for all patients. This program will cover the nursing services section in the hospital CoP manual. Facilities with Deemed Status accredited by the Joint Commission, Health Care Facility Accreditation Program, CIHQ, and DNV Healthcare must also follow these regulations.
There were some changes to the hospital nursing chapter of the conditions of participation (CoPs) in 2020. However, many of those changes are still awaiting interpretive guidelines and survey procedures.
This program will discuss the often-cited areas of the CoP manual involving nursing care: plans of care, staffing, policy changes, when a RN is required in an outpatient department, documentation, supervision, nursing leadership, verbal orders, and more. Nursing services has been cited over 7,200 times according to the most recent report.
Other changes in the past to the Nursing section include timing of medications, standing orders, plan of care, verbal orders, blood transfusions, IV medication, self-administration of medications and drug orders.
This program will also reference other important sections that all nurses should be aware that are outside the nursing services section. Such sections include the revised discharge planning standards, revised history and physicals, visitation, restraint and seclusion and grievances, and Section 1557 and non-discrimination.
Objectives
- Recall that CMS has a section on nursing services that every hospital must follow even if accredited
- Describe the three different timeframes for which all medications must be administered
- Discuss that nursing care plans are a frequently cited area by CMS
- Recall the requirements for verbal orders
- Detailed Agenda
- Introduction into the CMS hospital CoPs manual
- CMS deficiency reports
- 2020 changes to Nursing section
- CMS memos of interest that impact nursing
- Insulin pens
- Infection control breaches
- Texting of orders
- Ligature risks
- Safe injection practices
- Humidity in the OR
- Conditions of Participation – Nursing
- Nursing Services and 24 hours services
- RN on duty – recent update
- Organizational chart and nursing
- Chief Nursing Officer (CNO) responsibilities & requirements
- Staffing and delivery of care
- 24-hour nursing services and supervision
- RN to evaluate to care of all patients
- Nursing care plans
- Changes to the plan of care
- Agency nurse requirements
- Medication administration
- Order required for all medications
- Protocols, standing orders, order sets
- Requirements for complete drug order
- Three medications timing changes
- Safe Opioid use
- Standing orders and protocols
- Verbal orders
- Blood transfusions and IV medications changes
- Reporting blood administration and medication errors
- Self-administered medications
- CAH Nursing requirements
Other Manual sections of importance to nursing
- Restraint and seclusion
- Medication policies
- Visitation
- Discharge planning revised standards
Additional Information that Impacts Nursing
- CDC resources on preventing healthcare acquired infections (HAI)
- ISMP safe injection practices
- Non-Discrimination, Interpreters, and section 1557
- Appendix and Resources
Who Should Attend?
- Chief nursing officer
- All nurses
- Nurse managers/supervisors
- Nurse educators
- Compliance officer
- Chief of medical staff
- Risk manager
- Patient safety officer
- Senior leadership
- Joint Commission coordinator
- Regulatory officers
- Physicians
- Audit staff
Webinar Information
- DURATION : 75
- DATE / TIME(EST) : APRIL 10, 2024 | 1:00 PM
- SPEAKER :
Share this event
Related products
-
Sale!

2025 Recoupment Relief: Strategies to Protect Your Healthcare Revenue By Thomas Force
$499.00 – $799.00 Select options -

Common Findings in Coding Audits
$199.00 – $349.00 Select options -
Nursing: CMS CoP Standards for Hospitals
$199.00 – $349.00 Select options -
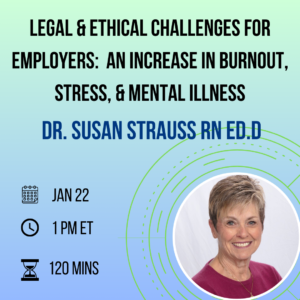
Legal & Ethical Challenges for Employers: An Increase In Burnout, Stress, & Mental Illness
$199.00 – $349.00 Select options